The Body Mass Index (BMI): Is it accurate?
There’s more to measuring fitness than gender, height and weight. Being FIT, no matter where you’re at in life, can be based on many more accurate methods. For years I have been telling people that the BMI is not an accurate indicator of health and fitness. As of late, I've seen some reputable sources quote the Body Mass Index as a way to gauge your health and fitness levels which I find laughable for several reasons. Most blatantly obvious is the fact that I'm considered borderline obese based on this index. Do you know what your BMI score is?
[caption id="attachment_674" align="aligncenter" width="351"]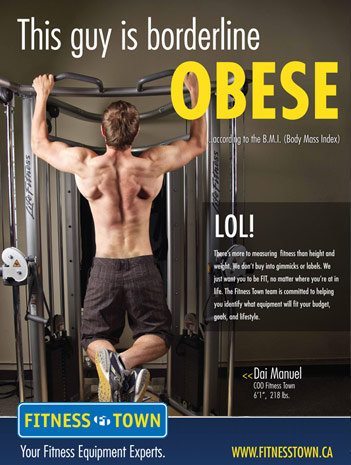 The BMI considers this guy borderline obese - what do you think[/caption]
The BMI considers this guy borderline obese - what do you think[/caption]
As we move into the 21st century, and the health and fitness of Western populations and populations throughout the world are getting worse, it is important that fitness consultants, experts, and doctors are able to accurately measure the health of the uninformed public. An inaccurate measure of health could promote negative self-esteem among the healthy and can lead them to pursue unnecessary diets. On the other hand, those who are unhealthy may be mislead to think they are completely healthy.
The most popular method of determining health and obesity is the Body Mass Index (BMI) due to its simplicity and affordability. BMI measurement ranges are separated into categories of severely underweight, underweight, average, overweight and three classes of obesity. BMI is calculated by dividing your weight in kilograms by your height in meters.
The problem with the BMI method is its inaccuracy in assessing individuals with a lot of muscle mass or a large frame. The BMI method loses much of its validity because it does not take into account one’s body composition including proportions of fat, water, bone, etc. As more and more health professionals and clinicians are using this method to assess the health of populations and individuals, we ask ourselves: how did we end up with such a faulty statistic?
History of BMI
 The formula first came up when Adolphe Quetelet published a study to define the “average man” in 1832. This study was not meant to determine obesity or obesity-related diseases. In his study, he found that a person’s weight varied not in direct proportion to a person’s height but the square of his height.
The formula first came up when Adolphe Quetelet published a study to define the “average man” in 1832. This study was not meant to determine obesity or obesity-related diseases. In his study, he found that a person’s weight varied not in direct proportion to a person’s height but the square of his height.
In the early 1900s, it was generally agreed by most medical professionals and organizations that people with too much adipose tissue (fat) were more likely to develop diabetes, hypertension, and other coronary heart diseases. Large scale studies were being carried out by health researchers and insurance companies throughout the century. It wasn’t until 1972 when Ancel Keys published his “Indices of Relative Weight and Obesity” to examine which height to weight formula correlated best with body fat %, that he found out the best indictor came from Quetelet’s formula, which Keys renamed the “Body Mass Index.” However, Keys warned against using this formula for individual diagnoses as the equation ignores individual factors like gender, age, body composition and how BMI affects health.
Limitations
One major shortcoming of the BMI equation is that it is over-simplistic. The formula is derived from population studies and the majority of people today lead very sedentary lives. Therefore, BMI assumes a lower lean body mass and higher relative fat or adipose content for the average person. This error in calculation leads to an overestimation of adiposity in people with a greater lean (fat-free) mass like muscled athletes. Likewise, BMI calculations underestimates adiposity on individuals with lower lean body mass like the elderly.
A further shortcoming is related to aging. As one ages and gets shorter and their weight stays the same, their BMI will actually increase. The standard BMI chart does not apply to everyone. Separate BMI charts and standards are needed for special populations. The BMI classifications for a “healthy” person are different for children and people who live in different countries.
In an analysis of over 40 studies involving a sample size of over 250,000 people, it was found that those with a lower BMI (<20) showed a greater risk of death from cardiovascular disease than people who were classified as normal (BMI 20-24.9). People classified as “overweight” (BMI 25-29.9) had the lowest incidence of total mortality and cardiovascular mortality. This study concluded that BMI is a poor evaluator and predictor of cardiovascular mortality. Their findings show that BMI fails to differentiate between body fat and lean mass.
Conclusion
While the BMI may be an okay indicator for large populations in epidemiological studies, it should never be used to diagnose individuals. There are many better clinical applications that can be used to assess body composition and health. The waist to hip ratio, waist girth measurements, and body composition analysis using dual energy x-ray absorptiometry (DEXA) or other methods are far more accurate techniques to evaluate a person’s health and fitness.
[divider style="solid" top="20" bottom="20"]
[caption id="attachment_674" align="aligncenter" width="351"]
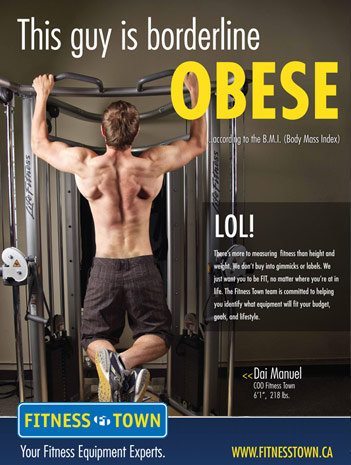 The BMI considers this guy borderline obese - what do you think[/caption]
The BMI considers this guy borderline obese - what do you think[/caption]As we move into the 21st century, and the health and fitness of Western populations and populations throughout the world are getting worse, it is important that fitness consultants, experts, and doctors are able to accurately measure the health of the uninformed public. An inaccurate measure of health could promote negative self-esteem among the healthy and can lead them to pursue unnecessary diets. On the other hand, those who are unhealthy may be mislead to think they are completely healthy.
The most popular method of determining health and obesity is the Body Mass Index (BMI) due to its simplicity and affordability. BMI measurement ranges are separated into categories of severely underweight, underweight, average, overweight and three classes of obesity. BMI is calculated by dividing your weight in kilograms by your height in meters.
The problem with the BMI method is its inaccuracy in assessing individuals with a lot of muscle mass or a large frame. The BMI method loses much of its validity because it does not take into account one’s body composition including proportions of fat, water, bone, etc. As more and more health professionals and clinicians are using this method to assess the health of populations and individuals, we ask ourselves: how did we end up with such a faulty statistic?
History of BMI
 The formula first came up when Adolphe Quetelet published a study to define the “average man” in 1832. This study was not meant to determine obesity or obesity-related diseases. In his study, he found that a person’s weight varied not in direct proportion to a person’s height but the square of his height.
The formula first came up when Adolphe Quetelet published a study to define the “average man” in 1832. This study was not meant to determine obesity or obesity-related diseases. In his study, he found that a person’s weight varied not in direct proportion to a person’s height but the square of his height.In the early 1900s, it was generally agreed by most medical professionals and organizations that people with too much adipose tissue (fat) were more likely to develop diabetes, hypertension, and other coronary heart diseases. Large scale studies were being carried out by health researchers and insurance companies throughout the century. It wasn’t until 1972 when Ancel Keys published his “Indices of Relative Weight and Obesity” to examine which height to weight formula correlated best with body fat %, that he found out the best indictor came from Quetelet’s formula, which Keys renamed the “Body Mass Index.” However, Keys warned against using this formula for individual diagnoses as the equation ignores individual factors like gender, age, body composition and how BMI affects health.
Limitations
One major shortcoming of the BMI equation is that it is over-simplistic. The formula is derived from population studies and the majority of people today lead very sedentary lives. Therefore, BMI assumes a lower lean body mass and higher relative fat or adipose content for the average person. This error in calculation leads to an overestimation of adiposity in people with a greater lean (fat-free) mass like muscled athletes. Likewise, BMI calculations underestimates adiposity on individuals with lower lean body mass like the elderly.
A further shortcoming is related to aging. As one ages and gets shorter and their weight stays the same, their BMI will actually increase. The standard BMI chart does not apply to everyone. Separate BMI charts and standards are needed for special populations. The BMI classifications for a “healthy” person are different for children and people who live in different countries.
In an analysis of over 40 studies involving a sample size of over 250,000 people, it was found that those with a lower BMI (<20) showed a greater risk of death from cardiovascular disease than people who were classified as normal (BMI 20-24.9). People classified as “overweight” (BMI 25-29.9) had the lowest incidence of total mortality and cardiovascular mortality. This study concluded that BMI is a poor evaluator and predictor of cardiovascular mortality. Their findings show that BMI fails to differentiate between body fat and lean mass.
Conclusion
While the BMI may be an okay indicator for large populations in epidemiological studies, it should never be used to diagnose individuals. There are many better clinical applications that can be used to assess body composition and health. The waist to hip ratio, waist girth measurements, and body composition analysis using dual energy x-ray absorptiometry (DEXA) or other methods are far more accurate techniques to evaluate a person’s health and fitness.
[divider style="solid" top="20" bottom="20"]




































































































